In today’s complex healthcare billing environment, the term pecos — referring to the Provider Enrollment, Chain, and Ownership System (PECOS) system — is being heard more and more. At Icon Billing LLC (www.iconbilling.com), we’ve seen firsthand how mis‑steps with pecos can lead to claim denials, delayed reimbursements and operational headaches. In this article we’ll dive deep into pe-cos: what it is, why it matters, how your practice can get it right, and how ignoring pecos can cost you dearly.
What is pecos?
The system called pe-cos is managed by the Centers for Medicare & Medicaid Services (CMS) and stands for Provider Enrollment, Chain, and Ownership System.
What pe-cos does is allow providers or suppliers to enroll with Medicare, revalidate, report changes, withdraw if needed, and generally maintain their enrollment status electronically.
In short: if your practice or your providers bill Medicare, maintaining your PECOS status is non‑negotiable.
Why pecos is critically important for medical billing
When you understand the role of pecos, you realize its significance:
-
If a provider doesn’t have a valid PECOS enrollment record, Medicare claims may be denied.
-
The system supports real‑time tracking and updates of provider data, which helps reduce errors.
-
Since some services can only be billed if the ordering/referring provider is enrolled in pe-cos, missing that can block downstream billing entirely.
-
From a compliance perspective, pe-cos helps providers meet regulatory requirements under Medicare, and failure to keep up can expose the practice to risk.
At Icon Billing LLC, we advise our clients early and often to verify pe-cos status before submitting claims to prevent denials, cash‑flow disruptions and audit issues.
How to enroll in pecos
Here’s a step‑by‑step overview of how to enroll in pe-cos:
-
Gather required credentials: National Provider Identifier (NPI), state license info, corporate/legal details (for groups or suppliers).
-
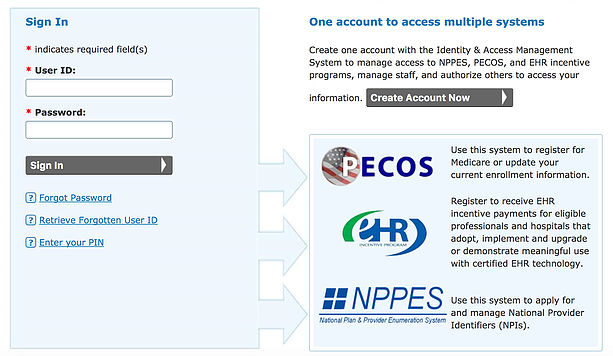
Log into the pe-cos portal via CMS’s “Internet‑based pe-cos” system.
-
Complete the enrollment application (initial, change of information, reassignment, etc.) via pe-cos.
-
Electronically sign, submit and track status through the portal.
-
Once approved, ensure the provider record in pe-cos is kept up to date (change of ownership, location, specialty, etc.). Failure to update may result in deactivation of enrollment privileges.
Common mistakes practices make with pecos (and how to avoid them)
Even experienced practices stumble on some pe-cos pitfalls. Here are frequent errors and how we at Icon Billing LLC help clients sidestep them:
-
Missing or incorrect NPI: If the provider’s NPI is missing from the pe-cos record or the NPPES data doesn’t match, claims may be rejected.
-
Out‑of‑date ownership or location information: When a practice moves, merges or changes ownership, the pecos record must reflect that. Otherwise, claims can be flagged.
-
Providers listed but not enrolled: Some think that because the provider is active medically they’re automatically in pecos. That’s not the case. Without proper enrollment they cannot bill Medicare.
-
Failure to re‑validate: The pe-cos system requires periodic revalidation. Ignoring that can lead to suspension of billing privileges.
-
Underestimating the pe-cos connection to billing: Some practices treat pe-cos as an “administrative” task and do not integrate monitoring of pe-cos status into their billing workflow. That’s a mistake.
By integrating pe-cos verification into pre‑billing checklists and our revenue cycle management workflow, Icon Billing LLC ensures that billing issues tied to pe-cos are flagged early.
The benefits of getting pecos right
When your practice is fully compliant with pe-cos, you’ll enjoy:
-
Fewer denied Medicare claims and faster reimbursements
-
Greater confidence that providers are properly enrolled and eligible to bill
-
Better audit readiness and reduced risk of compliance issues
-
Improved credentialing and provider onboarding efficiency
-
Streamlined change-of‑ownership, location or reassignment updates
In short, the effort you invest in managing pe-cos pays off in smoother billing, stronger revenue cycle performance and less administrative friction.
What happens if you neglect pecos?
Let’s be frank: ignoring pe-cos invites serious consequences. These include:
-
Claim denials: If a provider’s enrollment in pe-cos is inactive or invalid, Medicare will reject claims.
-
Delayed payments: Even if claims are eventually approved, delays in enrollment or validation can push reimbursement far beyond your standard.
-
Compliance risk and audits: Regulators increasingly examine enrollment verification via systems like pe-cos. Gaps in your PE-COS record can raise red flags.
-
Operational disruption: For example, if a practice fails to update provider status or location in pe-cos, they may be cut off from billing for certain services or equipment.
At Icon Billing LLC, we’ve seen practices suffer months of revenue loss simply because a key provider’s pe-cos enrollment expired and no one noticed until hundreds of claims were denied. This is why we emphasize pe-cos as part of our billing compliance process.
Integrating pecos into your revenue cycle strategy
Here are practical ways to make pe-cos an ongoing part of your billing and revenue cycle strategy:
-
Establish a pe-cos enrollment tracker: Maintain a spreadsheet or software module listing each provider, NPI, enrollment date, re‑validation due date, ownership/locations, etc.
-
Pre‑billing checks: Before submitting Medicare claims, verify the provider’s pe-cos status (active, validated, correct NPI).
-
Change‑management workflow: When a provider joins/leaves the practice, moves, changes specialty or ownership, trigger a pe-cos review/update.
-
Utilize billing partner oversight: If you outsource billing (such as Icon Billing LLC provides), ensure your billing partner monitors pe-cos and alerts you to any red flags.
-
Educate your team: Administrative staff must understand pe-cos basics – not just the enrollment form, but the implications for claims.
-
Periodic audit: Audit your pe-cos records annually or semi‑annually to ensure nothing lapsed, and correct proactively.
By weaving pe-cos into the revenue cycle rather than treating it as a one‑time enrollment task, your practice avoids surprises and builds resilience.
How Icon Billing LLC supports pe-cos compliance
At Icon Billing LLC, we know that pe-cos isn’t merely a paperwork exercise—it’s a foundational element of your Medicare billing success. Here’s how we help:
-
We monitor your providers’ pe-cos enrollment statuses on your behalf, alerting you proactively if a provider is nearing a re‑validation deadline.
-
We integrate pe-cos status checks into our billing workflow, so claims from providers are only submitted when enrollment is current, reducing denials.
-
We assist practices in managing the documentation and updates required for pe-cos (e.g., applications, change of ownership, location, reassignment).
-
We offer training and support so your administrative team understands the impact of pe-cos on revenue cycle management.
-
We provide strategic consulting if you are adding new providers, merging practices or expanding services – we guide you through the pe-cos implications.
With Icon Billing LLC’s support, you’ll have peace of mind knowing pe-cos‑related enrollment risk is actively managed.
Case study: How lack of pe-cos enrollment disrupted a practice
Consider this realistic scenario: A mid‑sized specialty practice brings on a new provider who begins seeing Medicare patients immediately. The provider’s NPI is active, but the pe-cos enrollment was never initiated. The billing department submits claims, and weeks later finds large volumes of denials citing “provider not enrolled in Medicare/pe-cos”. Revenue grinds to a halt while the provider must back‑track, complete a pe–cos enrollment, and wait for approval. In that interim the practice bears lost months of reimbursement, frustration from patients and staff, and unnecessary stress.
Had pe-cos been verified at onboarding, those issues would have been prevented.
FAQ about pe-cos
What type of providers must be enrolled in pe-cos?
Providers and suppliers billing Medicare (including physicians, nurse practitioners, clinical psychologists, DMEPOS suppliers) must enroll in pe-cos.
Is pe-cos enrollment mandatory?
While you may still submit paper enrollment via CMS‑855 forms, the online pe-cos system is highly recommended and some services require active pe-cos enrollment for claims eligibility.
How often does pe-cos enrollment need revalidation?
Enrollment records typically require periodic re‑validation every 3‑5 years or sooner if state or federal rules change.
What happens if my provider’s pe-cos enrollment lapses?
Claims may be denied, reimbursements delayed and the provider may lose eligibility to bill Medicare for certain services.
Can changes in ownership or location affect pe-cos?
Absolutely. Change of ownership (CHOW), additional practice locations, or changes in reassignment of benefits all must be updated in pe-cos to avoid disruptions.
How can I check my provider’s pe-cos status?
Via the pe-cos system you can check enrollment status; some MACs also provide lookup tools. It’s wise to verify before submitting claims.
Conclusion
The good news is that pecos is eminently manageable — but only if you treat it as integral to your billing operations rather than a one‑off enrollment task. At Icon Billing LLC we emphasize the ongoing monitoring, workflow integration and provider onboarding discipline required to keep pe-cos in good standing. By doing so, your practice avoids denied claims, cash‑flow disruptions and compliance risk. And the result? A smoother revenue cycle, fewer surprises and more time to focus on patient care instead of chasing enrollment issues. If you haven’t revisited your pe-cos status lately — now’s the time.